Health Disparities & Social Vulnerability
This area examines health disparities and social vulnerability, its use as a risk stratification tool, and conducts studies on health disparities in different populations.
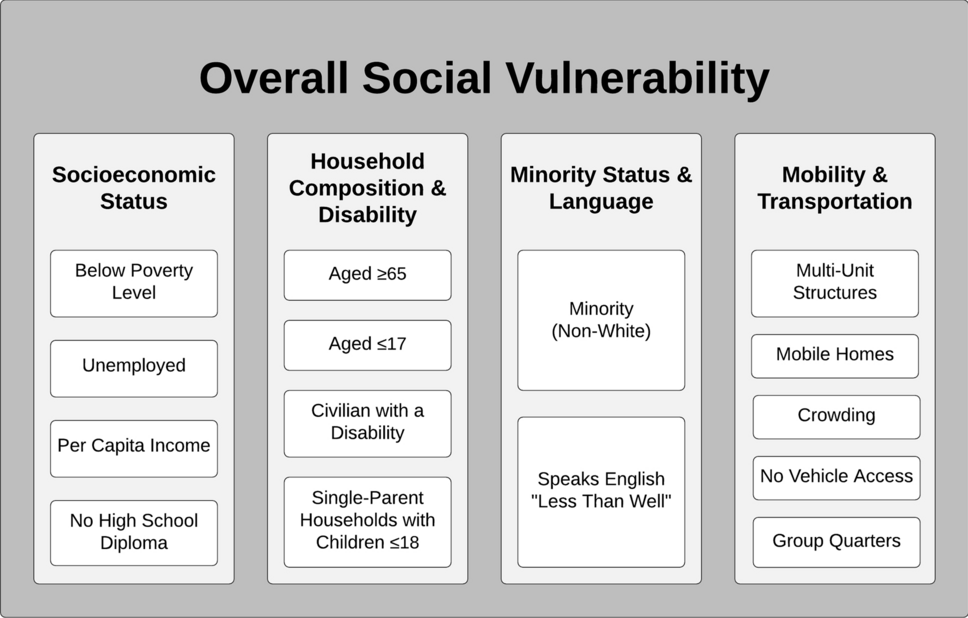
We explored the application of the Social Vulnerability Index (SVI), a composite measure by the Centers for Disease Control and Prevention, in oncology research using a systematic review. Searching five databases up to 13 May 2022, we identified 31 studies that applied the SVI to cancer patient outcomes. These studies spanned the cancer care continuum, from exposure to end-of-life care, with 15 focusing on mortality disparities. Our findings suggest that the SVI is a valuable tool for uncovering place-based disparities in oncology, potentially guiding targeted interventions to reduce cancer morbidity and mortality at the neighborhood level. (Check our publication: The social vulnerability index as a risk stratification tool for health disparity research in cancer patients.)
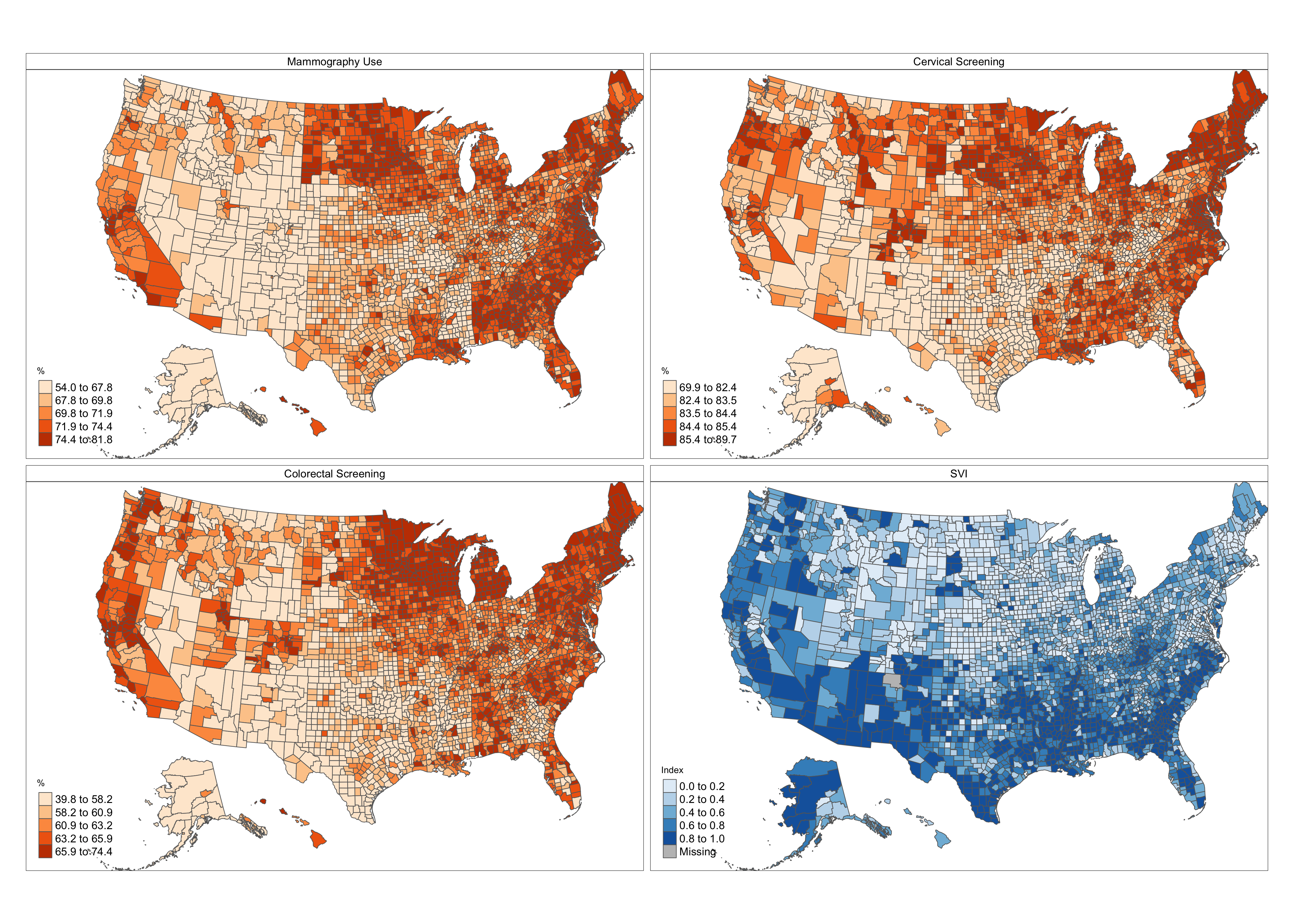
We investigated the geographic differences in breast, cervical, and colorectal cancer screening rates in the US and their association with county-level Social Vulnerability Index (SVI). Our findings revealed regional disparities in screening rates across counties. A higher SVI was linked to decreased odds of cancer screening, especially in counties with the highest vulnerability. After adjusting for factors like urban-rural status and insurance coverage, the association remained but was slightly weaker. This study underscores the importance of understanding how social vulnerability influences cancer screening rates, which can guide targeted interventions to address cancer prevention disparities. (Check our publication: County-level social vulnerability and cancer screening rates in the United States.)
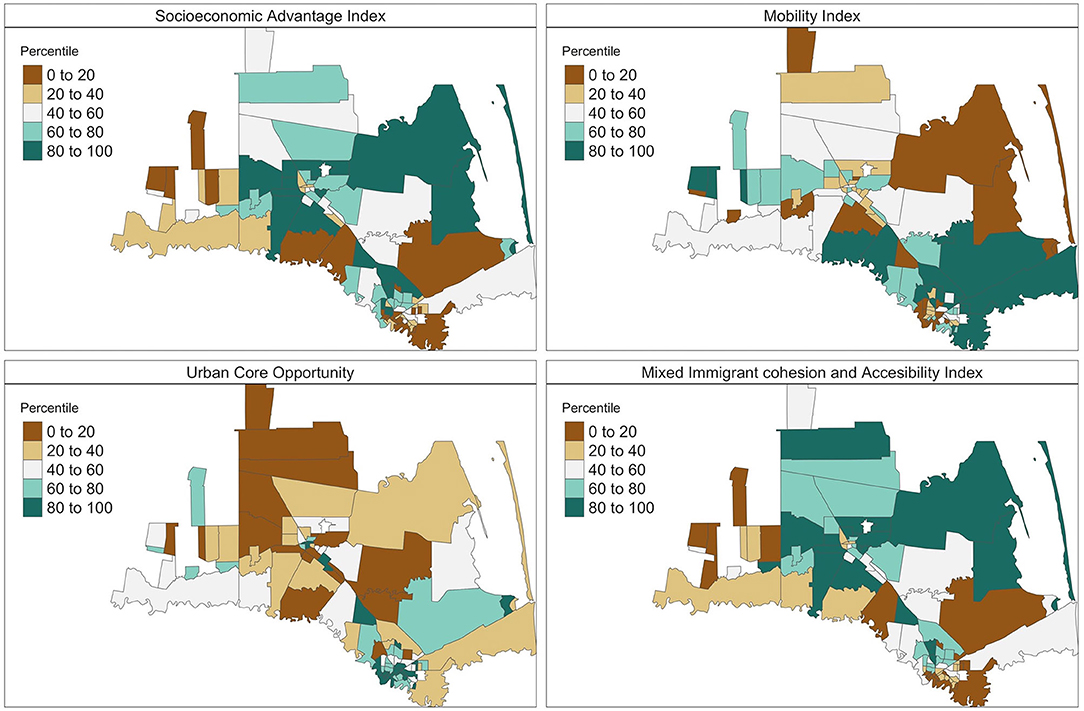
In the Lower Rio Grande Valley of Texas, diabetes is prevalent among Mexican Americans. We analyzed data from 1,568 participants in the Salud y Vida program to understand the influence of individual and community social determinants of health (SDOH) on diabetes management. Using Bayesian multilevel spatial models, we found that factors like older age, marital status, and language proficiency impacted hemoglobin A1C (HbA1C) reduction. Additionally, community SDOH, especially socioeconomic advantage, played a significant role. Our pioneering study highlights the need to incorporate community insights into diabetes interventions. (Check our publication: Individual and community social determinants of health on diabetes management in a Mexican American population.)